With Resources
Welcome to Visions Outreach
Trusted Leader in Supportive Services for Past Military Personnel and Families.
“Partner with national organizations to support military families and create a sustainable future for those who served.”
“Promote self-sufficiency and sustainability for military personnel and their families by partnering with national organizations and agencies.”
We will never leave vets behind
Giving Back to Those Who Gave So Much. Here are a few areas and ways Visions Outreach can help.
Helping With Mental Health
Helping whistleblowers
Helping Before Military Service
Helping After Military Service
Helping After Military Service
Talk With Us
Mon
Fri to Sat
Sun
Closed
We Care About You
PTSD AND HEALTH BENEFITS
PTSD
At Visions Outreach, we understand that PTSD and other mental health issues can have a profound impact on the lives of our veterans and their families. That’s why we offer a range of supportive services, including counseling, therapy, and resource connections to help our veterans cope with the challenges they face. We’re here to support you on your journey to healing and help you regain control of your life.
Military health benefits
We help you with finding benefits that provide service members and their families with access to quality medical care at little or no cost. This includes preventative care, primary care, specialty care, mental health services, and more. These benefits are an important part of supporting the health and well-being of those who have served our country, and ensure they can receive the care they need to live happy, healthy lives.
How We Help Whistleblowers
Whistleblowers
Visions Outreach provides comprehensive support to whistleblowers who courageously come forward to expose wrongdoing. Our initiatives include legal assistance, protection programs, counseling services, and advocacy. We understand the risks whistleblowers face and are committed to ensuring their safety, protecting their rights, and assisting them throughout the process. Our dedicated team works tirelessly to provide the resources and support whistleblowers need to navigate the challenges they encounter. At Visions Outreach, we believe in the power of whistleblowers to create positive change and we are here to stand by their side every step of the way.
How We Help before Military Service
Visions Outreach can provide several initiatives to help individuals before they enter military service. These include offering educational resources, mentoring and coaching, financial assistance, mental health support, and family support. By providing these services, Visions Outreach can help young people make informed decisions about their future, develop the necessary skills and knowledge to succeed in the military, and prepare for the challenges and opportunities of military life.
HOW WE HELP during MILITARY SERVICE
Visions Outreach can help military personnel during their service in several ways. This includes offering mental health support, family support, career development programs, financial assistance, and legal assistance. Military service can be stressful and challenging, and Visions Outreach can provide valuable resources and support to help military personnel and their families navigate these challenges. By providing these services, Visions Outreach can help military personnel achieve their personal and professional goals, maintain their mental health and well-being, and successfully navigate the unique challenges of military life.
HOW WE HELP After MILITARY SERVICE
Emergency?
The Reality Veterans Face
Hard Facts
During Facts
Before Facts
After Facts
Frequently Asked Questions
What is Visions Outreach?
Who is eligible for Visions Outreach services?
Visions Outreach serves all veterans, regardless of their branch of service, rank, or discharge status. We also offer support to military families and caregivers.
How can I access Visions Outreach's services?
You can access Visions Outreach’s services by contacting us through our website or by phone. Our staff and volunteers will work with you to determine your needs and provide you with the appropriate resources and referrals.
Is there a cost for Visions Outreach services?
No, all of our services are provided to veterans and their families free of charge.
How is Visions Outreach funded?
We are a non-profit organization funded through donations from individuals, corporations, and grants from government agencies. All donations go directly towards supporting our initiatives and helping veterans and their families.
Can I volunteer with Visions Outreach?
Yes, we welcome volunteers to help support our initiatives and make a difference in the lives of veterans and their families. Contact us to learn more about volunteer opportunities.
SUPPORT OUR VETERANS

Bronze Sponsorship
Tax Deductible
Bronze Level Sponsor, simply donate between $5 and $499.

Gold Sponsorship
Tax Deductible
Gold Level Sponsor, simply donate between $500 and $999.

Platinum Sponsorship
Tax Deductible
Platinum Level Sponsor, simply donate $1000 or More.
THANK YOU
Past and Current Sponsors
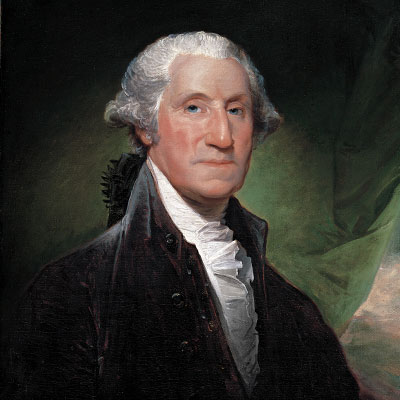
THEIR PROFOUND WORDS
Still True Today
Make a Difference
“Volunteer Opportunities with Visions Outreach”
As a volunteer, you can make a real difference in the lives of those who have served our country. Whether you’re helping to organize an event, providing administrative support, or working directly with veterans and their families, your time and effort will have a meaningful impact.
We welcome volunteers of all backgrounds, and we are committed to providing a safe, welcoming, and inclusive environment for all. If you’re interested in getting involved and making a difference, we would love to hear from you. Contact us today to learn more about how you can help support our veterans and their families through volunteering.